Using audio-visual vignettes to explore how nurses make the decision to restraint delirious patients on the critical care unit
How do nurses make the decision to restrain a delirious patient? What influences their decision? Do they follow protocols or base their decision on an individual assessment of the patient? If they assess the patient, what impacts on this process: the nurse’s experience, the acuity of the unit, or perhaps just how they felt that day? These are some of the questions I am seeking to answer through my PhD research.
My background research showed that nurses were the main decision makers when managing patient agitation and lacked support from medical colleagues. The literature suggests that nurses found caring for agitated and delirious patients physically and emotionally challenging. Nurses used negative subjective terms such as ‘mad’ and ‘poorly behaved’ to describe patient behaviours associated with hyperactive delirium despite the existence of objective, validated tools such as RASS and CAM-ICU. This can lead to the sharing of judgements of dysfunctional or deviant patient behaviour (Carveth, 1995). Wide variations in restraint use appear to be influenced by previous adverse clinical experiences and unit custom rather than evidence based practice.
| What is delirium? Delirium is a rapid onset, reversible, fluctuating condition characterised by inattention, changes in cognition, disordered sleep-wake cycle and increased or decreased psychomotor activity (American Psychiatric Association, 2013). It affects approximately 20-50% of mechanically ventilated patients in critical care (Krewulak et al., 2018). Hyperactive delirium presents as psychomotor agitation, which is often cited as a rationale for initiating chemical and physical restraint in critical care despite a poor evidence base (Ai et al., 2018). |
Think aloud
To answer these questions, I wanted to develop a data collection method which would help me to understand how nurses make the decision to restrain a patient, and identify potential modifiable factors. I rejected direct observation because it risked disrupting clinical care and I decided against written scenarios as i doubted these could convey the clinical urgency of caring for an agitated patient. Together with my supervisors, I chose audio-visual vignettes, or short films with ‘Think Aloud’ as the data collection method. ‘Think Aloud’ aims to reveal the thought processes involved in making decisions by encouraging participants to vocalise their thoughts.
Developing the method
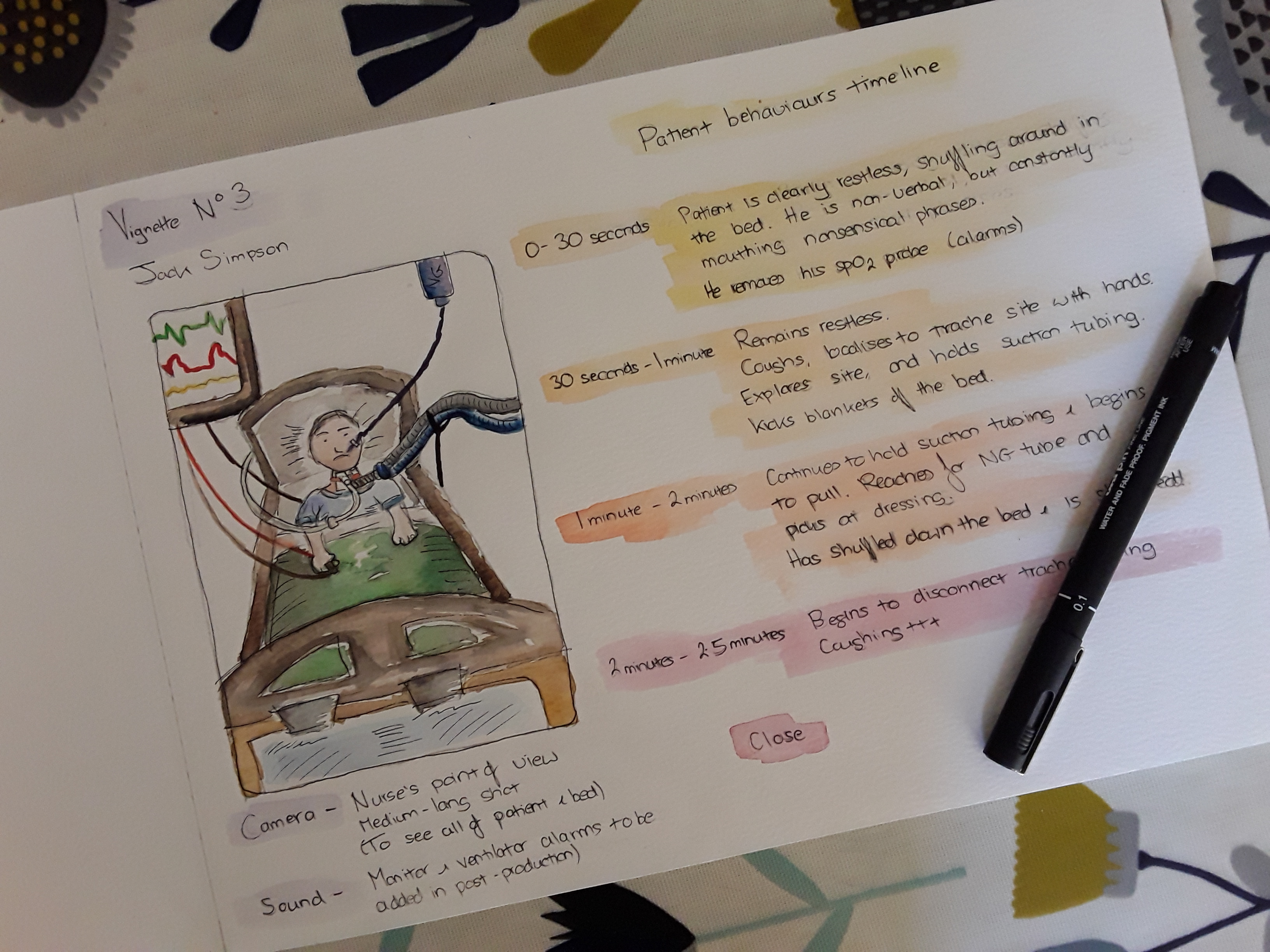
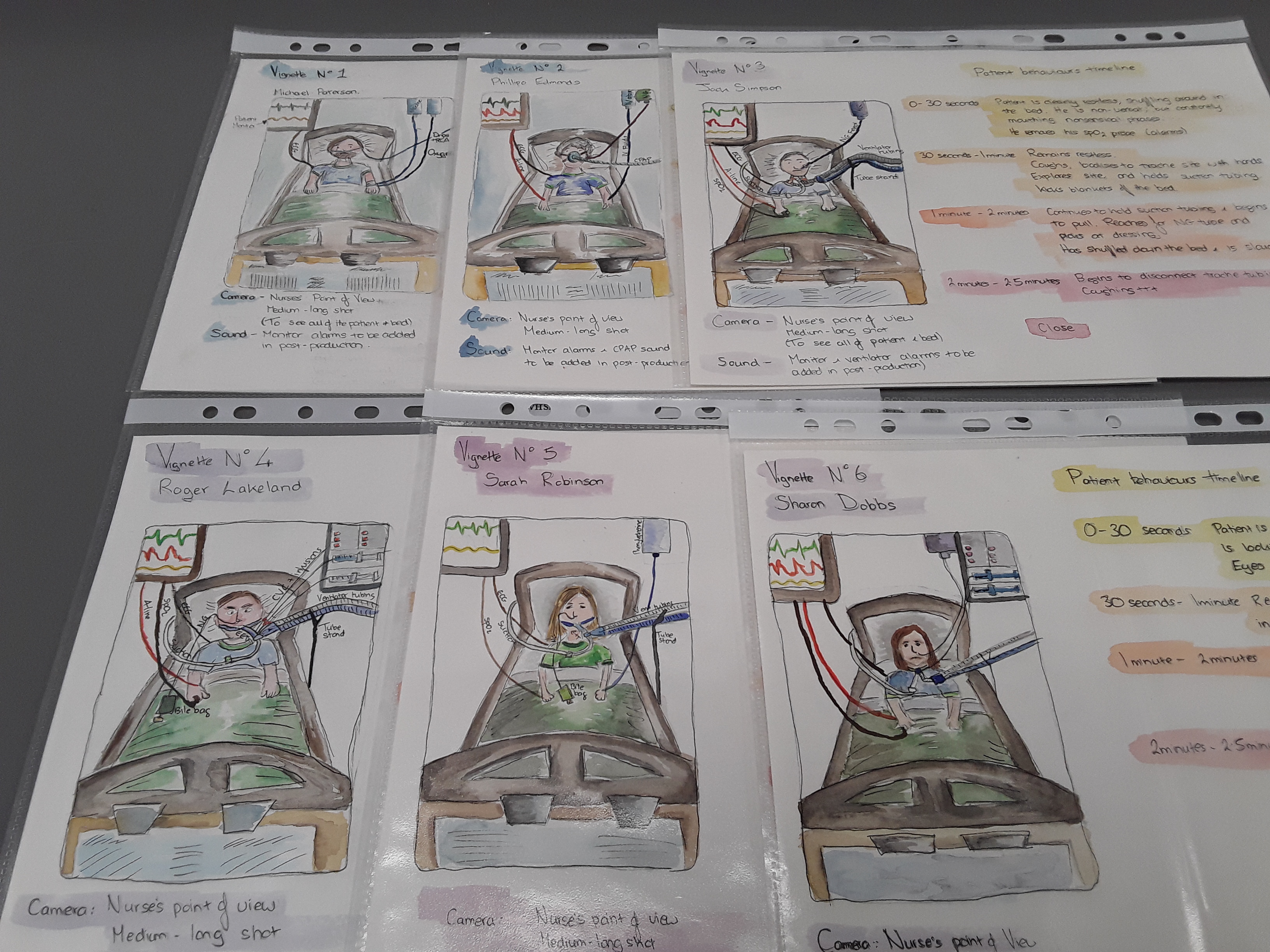
I began by writing scenarios based on my reflections on practice and cues identified from my background research. I asked a clinical expert (an Advanced Critical Care Practitioner) to check the scenarios before I developed illustrated storyboards that detailed the patient behaviours I wanted to ask participants about. An enthusiastic group of colleagues agreed to simulate these patient behaviours, and I filmed and edited the audio-visual vignettes early this year. The vignettes depict a range of delirious critical care patients with varying levels of potential risk inference, such as agitated or combative behaviour or the presence of medical devices. Each film is preceded by a verbal handover, which provides an opportunity to explore whether subjective descriptors influence how the participants perceived the patient and if this affected their decision-making.
I piloted the vignettes with three participants. The method works well and simulates decision-making under time-pressure in the critical care environment. Early data suggests variations in practice, and a focus on short-term management over a consideration of the long-term impact of restraint use.
For more information about my PhD research please visit my study page. Data collection is ongoing and the study is actively recruiting new participants.
Would you like to take part?
Your can contact me at a.m.teece@leeds.ac.uk. You can also follow me on Twitter @AngelaTeece
References
AI, Z.-P., GAO, X.-L. & ZHAO, X.-L. 2018. Factors associated with unplanned extubation in the Intensive Care Unit for adult patients: A systematic review and meta-analysis. Intensive & Critical Care Nursing, 47, 62-68.
AMERICAN PSYCHIATRIC ASSOCIATION, D. S. M. T. F. 2013. Diagnostic and statistical manual of mental disorders: DSM-5, Arlington, Va;London;, American Psychiatric Association.
CARVETH, J. A. 1995. Perceived Patient Deviance And Avoidance by Nurses. Nursing Research, 44, 173-178.
KREWULAK, K. D., STELFOX, H. T., LEIGH, J. P., ELY, E. W. & FIEST, K. M. 2018. Incidence and Prevalence of Delirium Subtypes in an Adult ICU: A Systematic Review and Meta-Analysis. Critical Care Medicine, 46, 2029-2035. 3